Don't Be So Sensitive
The outpatient at Redemption Hospital opens!
Right now in Liberia, the sensitivity of Ebola screening is a matter of life and death. In biostatistics
A highly sensitive screen means that if you get a negative result, you can be almost 100% sure that you can trust the result. At the height of the epidemic, West African health systems needed this kind of certainty. Even one undiagnosed Ebola patient passing through the system meant shutting down a hospital, killing a village, or closing down the airport.
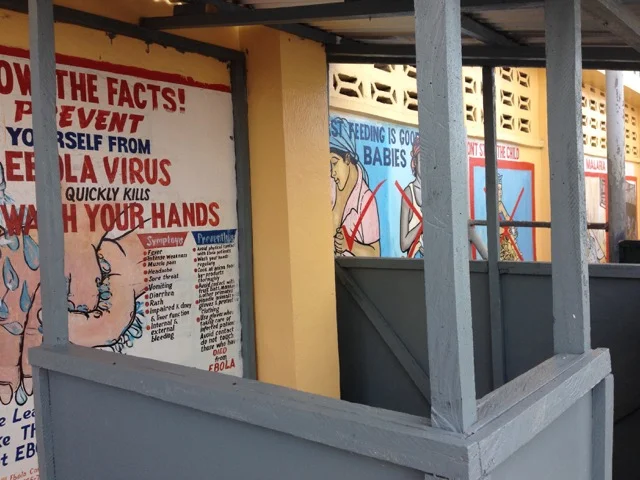
The trade off of high sensitivity is lower specificity. This means that you are casting the screening net so wide that you inevitably gather a lot of statistical seaweed. The equation for specificity is
Low specificity means that you are going to defacto get a significant number of false positive results. Lower specificity always comes with high sensitivity. Going back to the seafood analogy, a fisherman can’t expect to catch all the lobster possible with a single swoop of the net (high sensitivity/few false negatives) then be surprised to find non-lobsters in the pile (low specificity/some false positives).
High sensitivity-low specificity relationship is not a problem so long as you have the resources and time to deal with that mistakenly caught in the screen. You just run all the true and false positives through a different test specific to the pathology at hand, and determine who from whom. Doctors do this when diagnosing HIV. They use rapid tests that are extremely sensitive (you don’t want to miss a diagnosis). Following a positive test, they then run individuals through an Elisa PCR test very specific to HIV (before starting them on medicines). Any negative tests are confidently sent away with great relief, joy and alas, some explanation.
Finishing touches of Redemption rehabilitation
Time, resources and a different test. That is what is needed to reconcile highly sensitive screens in the real and statistical world. This is what is needed as Redemption becomes the first major hospital in Monrovia to reopen its doors next Monday after seven months of being shut. Other hospitals will be watching. There are currently only 20 available public hospital beds in all of Monrovia, a city with 2 million residents. Contrast this to the 480 Ebola Treatment Unit (ETU) Beds available country-wide, 450 which are free. The opening of Redemption will make available another 200 medical beds and if this goes well, lead to the reopening of JFK, JDJ, and partner private institutions as they witness the ability to practice medicine safely. But Redemption leadership is scared. They fear even one false negative Ebola case coming into the hospital. So they employ highly sensitive Ebola screening tools created during the height of the epidemic as opposed to screening tools more specific to the current context of rare infection with occasional local outbreaks.
Entrance to the planned triage path
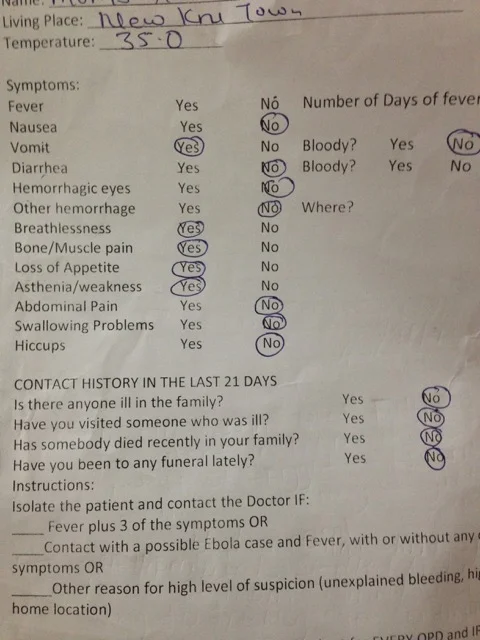
Screening criteria for Ebola includes fever + three symptoms (weakness, stomach, joint or swallowing pain, lack of appetite, shortness of breath, nausea, vomiting, diarrhea, and hiccups), or fever + bleeding or spontaneous abortion. This means on Monday, if the hospital doesn’t change course, the most common pathologies of malaria and bacterial pneumonia for children and sepsis and post-partum hemorrhage for birthing mothers will get caught in Redemption’s Ebola screening measures. Instead of being admitted and treated into Redemption for the ailment they most probably have, the system will instead divert these patients to Ebola Holding and Treatment Units across town to be tested for Ebola, which they probably don’t have. This will take anywhere from 8 hours to 1 day to get a result. This might sound attractive at a policy level or from the position of the bureaucrat, but not from the perspective of critically ill patients and the doctors and nurses caring for them.
To put the status quo into perspective, before the epidemic, Redemption received 800 patients each month to its pediatric and neonatal wards. If we assume a modest 25% would die without care, this means Redemption care prevented 200 deaths of children each month. For women, before the epidemic there were an average of 200 births a month at Redemption. Of these births 15% were complicated so approximately 30 maternal deaths were prevented.
Helpful case definition or anachronistic tool
Yet, with the current screening measures, nearly all of the above 800 pediatric patients and 200 maternal patients, will screen positive for Ebola. Febrile weak children with vomiting and diarrhea are the rule. Women in labor with bleeding and abdominal pain are the rule. These patients will be been sent to the ETU’s which are not be equipped to handle any of these medical emergencies. None of the ETU’s have oxygen, surgical capacity, ambubags, medicines requiring refrigeration, IV anti-malarials, delivery beds, feeding tubes or formula. ETU’s are not set up for treatment of non-Ebola patients. Any mortality rate is accepted in an ETU (at least you tried!). In short, 230 patients without Ebola who are suspected of Ebola will die as result of current screening measures. The irony is that the screening is supposed to prevent death.
Tomorrow the IRC with MSF partnering will use every skill we possess to convince the hospital director to change the screening criteria at Redemption for the opening next week. I recommend a focus on contact history and symptoms of vomiting, diarrhea and/or bleeding. Any patient with strong Ebola contact history and symptoms will be sent to an EHU or ETU according to the current standard. But within the cohort without clear contact history, any unstable patient who is dry (not vomiting, having diarrhea or bleeding), will get treated. Any unstable patient who is wet will also get treated but in a different area of the hospital by staff in full personal protective gear. Meanwhile, a test for Ebola will be sent locally. I say locally because testing capacity has recently been moved across town two hours away to the nearest empty ETU for reasons unknown to me. We must work to bring Ebola testing capacity right into the Redemption facility where it is most needed while carefully keeping track of patient hospital location and symptoms relative to Ebola status.
There does not exist a 100% sensitive and 100% specific test. There is only logic and reasonable risk in the transition between full-blown epidemics and tail-end of epidemics. It’s like jumping over something scary. Isn’t the reason always to get to a place less scary? You can only prepare by being certain of what you know and what you want to find on the other side. Bonus if it’s a human face.